ORIGINAL ARTICLES
Background. The problems of diagnosis, treatment and rehabilitation of patients with endometrial cancer (EC) remain relevant for the entire medical community. Radical surgical intervention shows high efficiency among the existing methods of EC treatment. However, it causes many complications that require rehabilitation support for patients. The development of new instruments and protocols for rehabilitation of EC patients is necessary.
Objective: to evaluate the effectiveness of comprehensive personalized rehabilitation program in patients after radical surgical EC treatment.
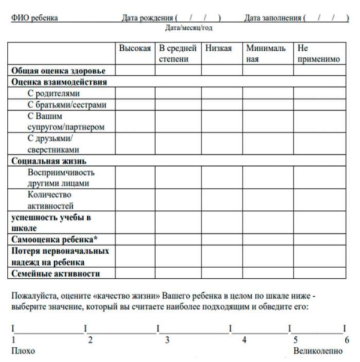
Material and methods. A prospective randomized comparative study included 61 patients with histologically verified stage IA endometrioid adenocarcinoma of high or moderate differentiation degree. The patients were divided into two groups: the group of “active” rehabilitation (n=29), and the group of “passive” rehabilitation (n=32). During 1 year, their physical, mental health and social engagement were assessed using questionnaires.
Results. The survey showed a low level of physical, functional, emotional and social well-being of EC patients at the first 3–7 days after surgery. After 12 months, a recovery in the quality of life of all participants was observed. However, patients undergoing “active” rehabilitation recovered significantly faster, and their quality of life was significantly higher compared to patients undergoing “passive” rehabilitation.
Conclusion. The obtained results indicate the effectiveness of a personalized approach in rehabilitation of EC patients. It is expected that its implementation will considerably reduce the incidence of complications and the burden on the healthcare system.
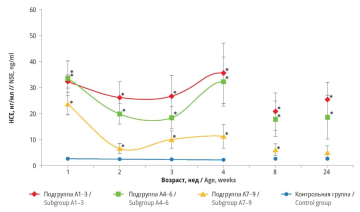
Background. Neuronal lesion, including hypoxic-ischemic damage to the central nervous system (CNS) in perinatal period, leads to the release of neuron-specific enolase (NSE) into peripheral bloodstream. Consequently, NSE can be considered as a biological marker of nervous system injury. Based on NSE level analysis, timely rehabilitation for newborns can be provided, thereby reducing the likelihood of complications associated with CNS injury.
Objective: retrospective assessment of NSE level in peripheral blood over a 24-week period in infants of different gestational age with perinatal hypoxic-ischemic CNS damage.
Material and methods. The study included 49 newborns who had suffered perinatal hypoxic-ischemic CNS lesion. Gestation period differed from 32 to 41 weeks. The control group consisted of 28 healthy full-term infants. NSE levels were measured using enzyme immunoassay. Patients of the main group were additionally divided into subgroups depending on Apgar scores at the 1st minute after birth, gestational age, as well as predominant CNS lesion – hemorrhagic with intraventricular hemorrhages or ischemic with periventricular leukomalacia.
Results. Throughout the observation period, NSE concentrations were inversely correlated with Apgar scores: lower Apgar indicators were associated with higher NSE levels. In addition, the subgroup of 32–33-week gestational age had significantly higher NSE concentrations compared with 34–36-week, 37–41-week subgroups, and control group. NSE levels in infants with periventricular leukomalacia were consistently lower than those in newbornes with intraventricular hemorrhage starting from the 1st week. Notably, a delayed increase in serum NSE concentrations was observed at the 4th week.
Conclusion. The obtained data indicate that blood-brain barrier permeability for NSE is preserved during perinatal hypoxicischemic CNS injury. Serum NSE concentration measurement can serve as a valuable tool in clinical practice for assessing the effectiveness of therapy at the stages of treatment and rehabilitation.
REVIEW ARTICLES
Background. In recent years, there have been significant changes in the regulatory documentation related to medical rehabilitation, caused by the need to consolidate the principles for rehabilitation of patients in post-COVID period and standardize the procedures used for it. Therefore, it is important to analyze the existing regulatory framework and the proposed changes that will come into force in the near future.
Objective: to assess the regulatory legal acts governing the provision of medical rehabilitation in Russia.
Material and methods. Regulatory legal acts and their drafts were obtained through the reference and legal systems “Kontur Standard”, “ConsultantPlus”, and the Federal Portal of Draft Regulatory Legal Acts. The following electronic libraries, databases and other sources were used to collect secondary information: eLibrary, Google Scholar, PubMed/MEDLINE, Yandex and social networks.
Results. Article 41 of the Constitution of the Russian Federation guarantees the right to health protection and medical care. Within the latter the use of medical rehabilitation can be considered. Going down to the next level, the term “medical rehabilitation” is found in Federal Law dated November 27, 2011 No. 323-FZ “On the fundamentals of health protection of citizens in the Russian Federation”. However, the requirements in the field under consideration are specifically described in Orders of the Ministry of Health of Russia No. 788n and 878n, which establish a three-stage provision of medical rehabilitation and give specific time instructions for the frequency and duration of care prcedures. The conditions for the transition of patients between the stages of medical rehabilitation are presented, and creating interdisciplinary rehabilitation teams is specified.
Conclusion. The analysis of innovations in the regulatory framework showed no fundamental changes in the regulation of medical rehabilitation. At the moment, there is a need to expand it by regulating the activities of multidisciplinary rehabilitation teams. A more detailed elaboration of normative documentation regulating the provision of medical rehabilitation to children is necessary.
Background. Hysterectomy is currently one of the most frequently performed surgical operations in obstetrics and gynecology, second only to cesarean section. However, such intervention is often associated with the risk of complications, including neurological ones. Neurological consequences, due to their characteristics, go beyond physical manifestations and exert psycho-emotional pressure on patients.
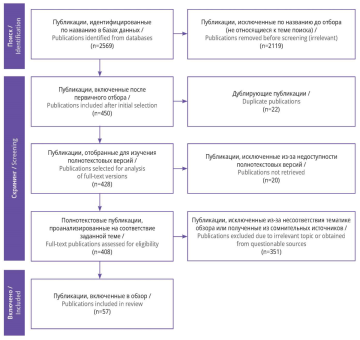
Objective: to determine the need for monitoring neurological manifestations in women undergoing rehabilitation after hysterectomy.
Material and methods. The search and selection of studies in Russian and English languages were conducted according to PRISMA recommendations in scientific databases and electronic libraries: PubMed/MEDLINE, ScienceDirect, Google Scholar, Microsoft Academic, DOAJ, eLibrary, CiberLeninka. In total, 2569 publications were revealed; after subsequent screening 57 articles were selected, which were devoted to the study of neurological adverse effects of hysterectomy and met all the screening criteria.
Results. Among all the neurological complications mentioned, the most common is chronic postoperative pain. It is detected in 30% of cases. At the same time, in the vast majority of cases, such pains are rare and are tolerated as mild discomfort. However, there is no unambiguous understanding of the nature of this complication. There is a theory about the essential role of estrogen production and substance P ratio in pain manifestations. Thus, a decrease in estrogen production with unchanged synthesis of substance P significantly reduces the pain threshold in patients, which is the cause of the observed chronic pain. A certain contribution to the formation of this neurological complication is made by residual ovarian syndrome, which is associated with incomplete removal of the ovaries during ovariectomy, traumatic neuroma and mononervopathy. Damage to the nerves or their plexuses in the pelvic area can cause intestinal and urinary disorders, leading to a decrease in the quality of life of patients. Excessive anxiety and depression are additional risk factors for the development of chronic pain after hysterectomy, and the accompanying postoperative changes often have a physical manifestation, for example, in the form of insomnia, restless legs syndrome and sexual dysfunction.
Conclusion. Hysterectomy is certainly an effective way to treat a number of gynecological diseases, but it often causes complications that require correction of the rehabilitation program. Neurological negative manifestations need special monitoring, since the depressive state of patients may lead to chronicity of pathological processes.
One of the most common gynecologic diseases is polycystic ovary syndrome (PCOS). The pathologic conditions caused by this syndrome require careful attention from not only gynecologists, but also therapists, endocrinologists, oncologists, cardiologists, and psychologists. The reproductive function of women with PCOS and associated infertility needs further careful study. At the same time, it is necessary to develop measures for the correction and prevention of all disorders associated with this pathology. The article describes the importance of multidisciplinary, comprehensive approach to PCOS patients, the need to study and implement rehabilitation means aimed at restoring all aspects of women's health, including after surgical treatment.
Background. Epilepsy is a common and persistent neurological disorder that typically affects children. In addition to the obvious physical and emotional outcomes for a child, epilepsy, like other chronic conditions, can have a profound impact on the well-being of family members. In order to comprehensively address and manage parental stress, it is essential to have a thorough understanding of the various factors involved.
Objective: to determine the influence of parental stress on the course of epilepsy in children.
Material and methods. A search for publications devoted to the study of parental stress in pediatric epilepsy in scientific databases PubMed/MEDLINE, Google Scholar, ScienceDirect, eLibrary identified 2670 articles. After the selection, 39 publications were included in the review.
Results. There are a number of questionnaires that allow determining the level of parental stress: PSI, PSI-SF, PIP, IPES. They have shown their accuracy and have been validated in studies devoted to parental stress in parents of children with chronic diseases, including epilepsy. The relationship between the level of parental stress and the prognosis of epilepsy course, psychological state of children and the quality of life of parents was shown. The need for additional psychological support for parents of children with epilepsy was indicated. The feasibility of using biomarkers of brain damage in children as an additional tool for assessing the severity of parental stress was presented.
Conclusion. Children with chronic conditions, such as epilepsy, and their families often face a number of interrelated problems. These include parental stress, difficulties in following treatment plans and adjusting to school, social discrimination. Despite the relevance of this issue, there are no large-scale, longitudinal studies examining stress in parents of children with epilepsy, so the relationship between epilepsy and parental stress is not fully understood. A collaborative approach is necessary, in which both the child and parents take responsibility for the treatment of the disease.
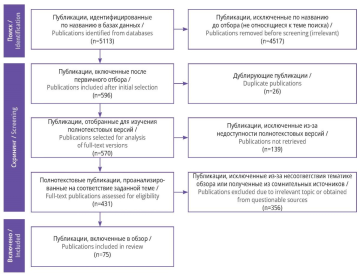
Background. In recent years, oncogynecological diseases have been diagnosed more frequently in women of reproductive age. Despite the high efficiency of treatment measures, significant shortcomings in the rehabilitation system for such patients are noted.
Objective: to present the continuity and features of the rehabilitation system for patients of oncogynecological profile.
Material and methods. This review included 75 relevant publications from authoritative sources that presented unique findings. The search was conducted in Russian and foreign online libraries, databases and search engines. PRISMA recommendations were used for search and screening.
Results. Oncogynecological patients need special attention in providing them medical care at the recovery stage. It is important to adhere to the principle of continuity between all steps of rehabilitation system: immediately after treatment, in rehabilitation department, and on outpatient stage. This system has been developed in Russia, but it needs scaling and solving a number of problems, ranging from a shortage of rehabilitation doctors, limited use of promising rehabilitation tools to insufficient provision of psychological assistance and the absence of generally accepted comprehensive rehabilitation system. At the same time, there is sufficient set of traditional and high-tech rehabilitation methods to provide highly specialized care.
Conclusion. Aggressive treatment of oncogynecological diseases has a detrimental effect on the general well-being of women, significantly reducing their quality of life. Previously, proper provision of rehabilitation care encountered the rigidity of the system both at methodological and administrative levels. Recently, there have been positive shifts in solving problems of providing care to oncogynecological patients, however, the presented measures are not enough to qualitatively change the situation.
ISSN 2949-5881 (Online)